Nurse Practitioners (“NP”) have been gaining increasing autonomy in their practice allowing them to practice without physician supervision in several states. Currently, twenty-seven states and Washington, D.C. allow NPs full autonomy to practice without physician supervision. Twelve states allow NPs to only perform some of their duties independently and eleven states still require NPs to work fully under physician supervision.
The passage of laws granting NPs more autonomy has led to confusion as to how this autonomy fits with traditional roles of the physicians and other providers in the practice of medicine. To clear up the misperceptions of the laws, we will examine the scope of practice of a typical NP, and distinguish the difference between a restricted practice and an autonomous practice.
What’s The Scope of Practice for A Nurse Practitioner?
In general, a NP is a registered nurse (“RN”) licensed by the relevant state’s nursing board to practice as an advanced practice registered nurse sometimes called an APRN. The NP’s scope of practice is based upon formal educational preparation, continued advanced practice experience and the accepted scope of professional practice of the particular specialty area. NPs are able to practice advanced nursing services within their selected population focus. When operating outside of their scope or on a patient outside of their chosen population focus, they typically operate under their RN scope of practice and limitations. The most common areas of NP certifications are family (70.3%) and adult-gerontology primary care (8.9%).
Early History
In 1965, Medicare and Medicaid coverage expanded, new people qualified for primary care coverage, and the resulting shortage of available physicians prompted the creation of the nurse practitioner profession. The first NP program was founded by Loretta Ford and Henry Silver in 1965 at the University of Colorado. By the early 1970’s, this certificate program had become a master’s degree program that was spreading quickly. By 1973, there were more than sixty-five NP programs in the United States.
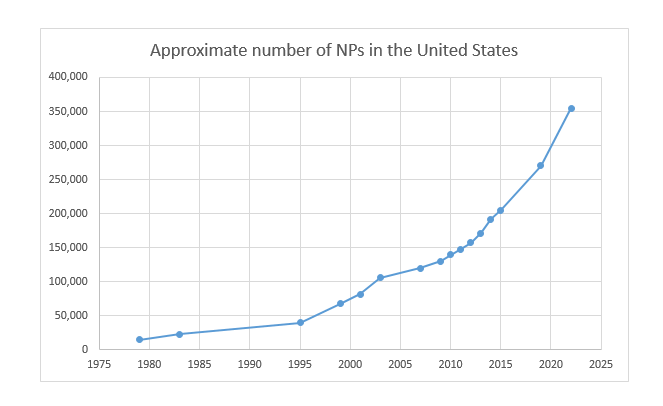
Despite this growth, the profession struggled for legitimacy. Encouragingly, the U.S. government had spent $100 million on nurse practitioner programs by 1987. However, the profession did not have provider status, rendering NPs ineligible for reimbursement. The profession was hindered, in part, by lack of standardization regarding certification and professional duties. It is important to note that in the midst of these issues and during its incipiency, the profession was growing rapidly as noted by the below charts developed by American Association of Nurse Practitioners.
Institutional Progress
From the late 1980’s to the turn of the century, the profession took significant steps forward. In 1989, limited reimbursement arrived through the Omnibus Reconciliation Act of 1989. The early 1990’s fiscal crisis in health care led to a decline in more traditional healthcare roles and a counterbalanced increase in NPs’ role. Additionally, NPs received direct reimbursement from the Balanced Budget Act of 1997. Finally, by 2000, all 50 states recognized NPs’ ability to legally practice.
The Road to Standardization
There has been a movement to incorporate NP education standards into the nursing accreditation process. The American Association of Colleges of Nursing (“AACN”) has sought to require a Doctor of Nursing Practice degree (“DNP”) for NPs since 2004. Progress towards widespread adoption of this policy has been slower than anticipated. However, DNP programs are now available in all fifty states plus the District of Columbia. Overall, the growth and demand for NPs has continued to rise. This trend is expected to continue as the percentage of the population 65 and older continues to increase.
Formal Education and Certification
A registered nurse typically becomes certified as a NP by the completion of a formal educational program. After that, an NP’s practice can often be expanded by other training or clinical experience. States take a varying view on how flexible such expansions can be: Texas, for example, has some allowance for expansion of practice but also has certain limits in place where only formal education is required. Other states seem to allow the scope of practice to include whatever the NP is able to learn and safely administer from actual experience. For example, Colorado requires a NP to submit a signed attestation to the nursing board stating the NP has completed at least three years of combined clinical work to obtain provisional prescriptive authority. The NP must then complete 750 hours of structured mentorship with a physician or advanced practice nurse in order to obtain full prescriptive authority. Finally, NPs are primary care providers, but they are required to have a focus, for example women’s health or family.
Prescriptive Authority
All states allow NPs some level of prescribing authority for controlled substances. In general, the NP usually needs to get a DEA number, register with the state’s prescribing system, and be authorized to prescribe by a physician or by their board. In states where there are restrictions, it is usually in a formulary, an official list of included or excluded drugs that they may prescribe, or authorized in a written practice agreement where a physician authorizes the classes of drugs they may prescribe. Some examples of States are as follows:
- Maryland provides for full prescribing authority with NP licensure;
- Missouri requires a Collaborative Practice Agreement (“CPA”) with a supervising physician; and
- Texas requires a written prescriptive authority agreement from a physician identifying the types or categories of drugs that may be prescribed.
To further complicate the prescriptive authority, when a NP is prescribing drugs for uses other than what the FDA originally approved, known as “off-label use”, they may have additional restrictions. For instance, Oklahoma maintains separate formularies for both physician assistants (“PA”) and NPs. Each formulary includes a list of drugs the licensees are prohibited from prescribing on their own. It is in these formularies where some off-label uses for certain drugs may be prohibited directly or indirectly by excluding entirely a class of drugs and not accounting for alternative uses. Additionally, the NP must work under a collaborative agreement with the supervising physician, but is then allowed to administer Schedule III-V controlled substances.
Restrictions on prescribing under “standards of care” are typically found in the statute that grants the prescribing rights to the NP. The prescription is usually worded to allow prescribing for approved uses unless certain requirements can be met. Usually, the requirements are that the off-label use is supported by studies or peer-reviewed and is included in the current standard of care for that ailment. For example, the Texas Board of Nursing’s administrative code limits NPs to ordering and prescribing medication only for FDA approved uses unless the use is part of an official trial or review board, or if the use is both supported by evidence-based research and within the current standard of care for treatment of that particular condition. While those carve-outs will allow Texas NPs to prescribe medications for many off-label situations, it limits them to only those mainstream off-label uses. NPs in Alabama have similar requirements to only prescribe off-label if it is part of the current standard of care, supported by evidence-based research, and approved by the collaborating physician. Based on these different levels of authority of NPs, medical facilities that have offices in multiple different states must implement safeguards to comply with these prescriptive authority laws.
Good Faith Exam/Initial Exam
In all states, prior to rendering medical services to a potential patient, an examination of the patient must be conducted to ensure that the patient is a good candidate for the procedures he or she is seeking. This is often referred to as the “Good Faith Exam.” The Good Faith Exam must be performed by a physician, PA, or NP. In every state where the NP has full practice authority, the NP may conduct this Good Faith Exam without any supervision of a physician. In states where the NP has a more restricted authority, this Good Faith Exam will be subject to their supervising or collaborating physician. As with most other NP attributes described in this article, there is a spectrum of existing regulation within the fifty states. Arizona allows NPs to examine patients and establish medical diagnoses. Similarly, Kentucky requires NPs to “conduct an examination” of the patient, and Oregon references “assessment” in describing the NPs’ role.
Ability to Delegate
Once the Good Faith Exam has been completed, the NPs can typically delegate to a RN. In some states, NPs may also delegate to Licensed Practical Nurses (“LPN”), and even unlicensed persons, sometimes referred to as unlicensed assistive personnel (“UAPs”), or medical assistants (“MAs”). The substance of what can be delegated varies widely from state to state. Some states allow NPs to delegate their advanced nursing functions. Other states only permit assignment of tasks that are already in the scope of practice of the RN or LPN and do not allow any delegation to UAPs or MAs. For example, in Texas, NPs do not have the same authority to delegate as physicians and are limited in their ability to delegate their role. The Texas Board of Nursing website provides a detailed explanation of what and to whom a NP can delegate.
Restrictions on NPs’ Autonomy
As mentioned above, NP’s are subject to a continuum of regulations, most of which require some level of interaction with a physician, with or without written agreements. Where an agreement is required, some states treat practice and prescription independently. Texas NP’s have independence in nursing practice, but not prescriptive authority (where they must have an agreement with a physician).
The level of supervision required can be categorized into two levels: (1) Supervised Practice; and (2) Collaborative Practice. The majority of states require some form of physician oversight for NP practices, while the less restrictive states are moving to a “collaborative” model, or reducing the formality of the supervisory relationship.
Supervised Practice
The most restrictive form of a NP practice is the supervised practice. A supervised practice approach is characterized by requiring a written supervisory agreement or protocol that sets the NP’s permitted scope of practice and prescriptive ability. States administering a supervised practice approach are in decline. Despite the decline, remaining state examples who utilize this practice include Oklahoma and California. For example, in California NPs are required to have a standardized procedure that is developed and approved by the supervising physician.
One subset of the supervised practice approach also requires approval by the relevant state’s nursing board. In Alabama and Georgia, a NP must file their credentials and certifications, demonstrating their capabilities prior to rendering any medical services. However, it is more common to only require the agreement be maintained at the practice site and available for review. These agreements often require the NP to practice as an employee of a physician or health care facility.
Collaborative Practice
A collaborative practice approach fills the middle ground between supervised and independent practices. For this reason, there is great variety among collaborative practice approaches. More restrictive collaborative practice approaches border on being supervised practice, while a permissive collaborative practice approach looks more like an independent practice. Naturally, most collaborative practice arrangements exist in the in-between.
The pertinent attributes that distinguish collaborative practices from one another are as follows: (1) the agreement needs to be in writing; (2) the agreement needs to be approved by the state board; and (3) various requirements regarding meetings with a supervisor, geographic location, or formal chart review. Because of the variance of requirements, the number of distinguishing factors makes collaborative practice the most fluid of the three approaches. For example, in Texas, the supervising physician cannot delegate to more than 7 full time equivalent NPs and PAs, or in Missouri, the collaborating physician and NP must be within 75 miles of each other.
Independent and Autonomous NP Practices
Independent practice is the most recent, broad development in the NP field. As states adopt independent practice for NP’s, the legislation can cause some confusion regarding NPs’ statutory scope of practice. In some states, the governing body repealed the need for a written agreement. States that take this approach can create a vacuum of insufficient guidance, which can result in friction between physicians and NPs as the lines between the fields become blurred. Wary of such issues, states that have made the move to independent practice more recently have provided a more structured statutory scope of practice. For example, in 2017, Illinois passed legislation which allowed NP’s to apply for full practice authority, effective January 2018. Unfortunately, there were no corresponding administrative rules on the process to obtain this license. As a result, this set off a firestorm of NPs starting their own independent practices in that State in 2018, even without any official guidance. On June 14, 2019, the much anticipated 68 page administrative rules were finally released. These final rules include filing fees and notarized attestations to the board of completion of the following: (1) 250 hours of continuing education and training in the NP’s area of certification and (2) at least 4,000 hours of clinical experience in their area of certification that is in collaboration with and certified by a physician(s). Additional continuing medical education, an Illinois controlled substance license, and a Federal Drug Enforcement Administration number are also required. These regulations do not change the rules for ownership of professional entities. As such, a NP cannot own, or jointly own, a medical practice with physicians. However, nothing prohibits a NP from owning a nurse practitioner professional practice, which is distinguishable from a medical practice. It would not be recommended that an NP market their practice as “med” or “medical” based on the IL advertising rules. It would more accurately be termed an “advanced nursing spa” or “aesthetic nursing practice”. As such, NP’s in IL that meet these rules will be autonomous from physicians, but still cannot own a medical practice.
Types of Independence
There are at least two approaches to define independent practices: (1) by virtue of being a licensed NP, or (2) through experience as an NP over time. Under the first approach, some states equate the act of being licensed as a NP with independent practice. For example, Nevada allows NP’s to practice independently and prescribe independently, except regarding Schedule II prescriptions. Authorization to prescribe Schedule II controlled substances require (a) two years or 2,000 hours of clinical experience, or (b) the NP provides prescription pursuant to a protocol approved by a collaborating physician.
Under the second approach, NP’s must practice under an agreement with a physician for a certain amount of time in order to gain independence. New York takes this approach, requiring 3,600 hours of NP practice before the physician agreement can be lifted and independence granted. In another variety, Virginia requires 9,000 hours or five years of practice before a NP can apply for autonomy.
However, NP independent practices may still have restrictions on prescriptive authority. Such a statute often contains authorized schedules and classes of drugs that are prohibited. Opioids are commonly restricted, as in Florida where only a seven-day supply of opioids can be prescribed. Alternatively, in some states the nursing board takes applications from NPs and grants approval for prescriptive authority, often predicated on the NP’s education or training.
Ownership
Most states define who may own a medical practice. This area of law can be extremely confusing, as these ownership statutes are not tied to the NP scope of practice laws. Some states that have passed independent practices for NP’s have also made it clear as to if a NP can own a medical clinic. However, in many states the business code governing ownership of a medical practice may require physician ownership or partial physician ownership even when a NP is independent. Basically, the corporate practice of medicine is a doctrine that requires any entity providing clinical medical services in that state to be a professional entity wholly owned by a licensed physician. This rule prohibits non-physicians from owning a medical practice or employing physicians. The concept is to prohibit a non-physician from making and controlling professional medical judgment. For example, in Texas a medical practice may only be owned by a physician, PA, or chiropractor, subject to a host of restrictions. However, the Texas Business Organizations Code allows any licensed individual to form a professional entity. For this reason, many NP’s and PA’s believe they can form a professional entity, own 100% of it, and practice medicine out of that professional entity. Although we are unaware of enforcement against a NP for owning a medical practice in Texas, interpretation of the applicable laws indicate that a NP may not own a medical practice in Texas. States like California are clearer as to NP restrictions on ownership, as a professional medical entity in California can be owned 51% by a physician and 49% by other licensed medical providers, subject to a host of restrictions.
To further confuse the issue, states like Ohio allow NP’s to own 100% of their medical practice, but still require the NP to have a written collaboration agreement with a practicing physician. As such, an entity wholly owned by a NP may still be subjected to supervision and prescriptive authority restrictions.
Contact ByrdAdatto for Assistance with NP Independence
The laws governing NP scope of practice vary greatly from state to state. It is important if you are an NP or a practice employing NP’s to stay abreast of your state’s laws and any changes occurring. At ByrdAdatto we are working hard to ensure our clients are up to date with the latest regulation and rule changes to maintain compliance. If you have any questions about this alert, contact ByrdAdatto at info@byrdadatto.com.
We are grateful for the significant research and drafting contribution to this article from our Law Clerk, Clint Nuckolls. Clint is a third-year student at SMU Deadman School of Law.
