Management services organizations (“MSO”) have been around for decades serving a multitude of purposes in health care. MSOs colloquially have been referred to as the duct tape for health care business arrangements by health care attorneys. They can fix many problems with a health care deal. When implemented correctly a MSO can be a successful vehicle for several different models, arrangements and reasons. However, if implemented incorrectly a MSO can lead to regulatory scrutiny and risk given the highly regulated health care industry.
This field guide is a five part series and will, after an introduction to the MSO, address in each part the differing uses that MSOs play in health care arrangements:
- Part 1 – What is a management services organization (MSO)?
- Part 2 – Corporate Practice of Medicine (CPOM) Uses
- Part 3 – Regulatory Uses
- Part 4 – Business Structuring Uses
- Part 5 – Exit Plan Uses
Corporate Practice of Medicine (CPOM) Uses
The MSO model, with proper set up and implementation, has long been the gold standard as the model used when non-physicians are involved in a health care arrangement. Addressing the laws prohibiting non-physicians from owning a medical practice, called the corporate practice of medicine (CPOM), is the first step towards understanding the functionality of the MSO model as a means to navigate CPOM.
What is CPOM?
Before answering the question “What is the corporate practice of medicine,” one must first acknowledge and address a root question: What is the practice of medicine? Asked another way: What qualifies as a medical service? Ultimately, this is the key to determining whether CPOM is even an issue. If the services provided by a business are not the practice of medicine, then it will not trigger a state’s CPOM laws. However, this determination is not always as easy as one thinks.
Most states define the practice of medicine broadly, resulting in many services that intuitively may seem non-medical qualifying as medical services. This has created confusion across the spectrum of elective and non-invasive medical services, including common services provided in medical spas, IV hydration bars, weight loss centers, wellness centers, and alternative medicine practices. Some states, like Texas, have enacted specific laws stating non-invasive services are in fact considered medical services (see the Texas CPOM Field Guide). Other states provide little to no guidance on the issue, furthering the confusion and leading to differing interpretations and opinions.
CPOM Doctrine
With this background in mind, the CPOM doctrine is a state law doctrine designed to require that only physician owned entities practice medicine, thus limiting the commercialization of medicine by non-physicians. The underlying purpose of the CPOM doctrine is to protect patients and preserve the integrity of the provision of health care by preventing undue influence on or interference with patient care. Stated differently, the CPOM doctrine, by restricting ownership of a medical practice to licensed physicians, attempts to ensure patient care is held to a standard established and controlled by physicians.
Where Does CPOM Exist?
CPOM varies across the country. CPOM can be created by statute, administrative rules, or case law and there are often complexities involved to ascertain the actual rule in a state as to ownership.
In an attempt to simplify how the CPOM rules are generally structured, there are three basic approaches states take to ownership of a medical practice:
- Physicians Only
- Physicians Plus Others (with Strings Attached)
- Anyone Can Own
Physicians Only
In these states, only physicians may own a business that provides medical services, eliminating the possibility of non-physician ownership entirely. New York, New Jersey, and Illinois are examples.
Physicians Plus Others (with Strings Attached)
In these states, physicians and non-physicians may jointly own a business that practices medicine if certain boundaries are in place to ensure that medical decision-making remains in the hands of physicians. Several states, including Texas, California, and Arizona, fall into this category.
Anyone Can Own
In these states, anyone can own a business that provides medical services. Florida and Virginia are examples.
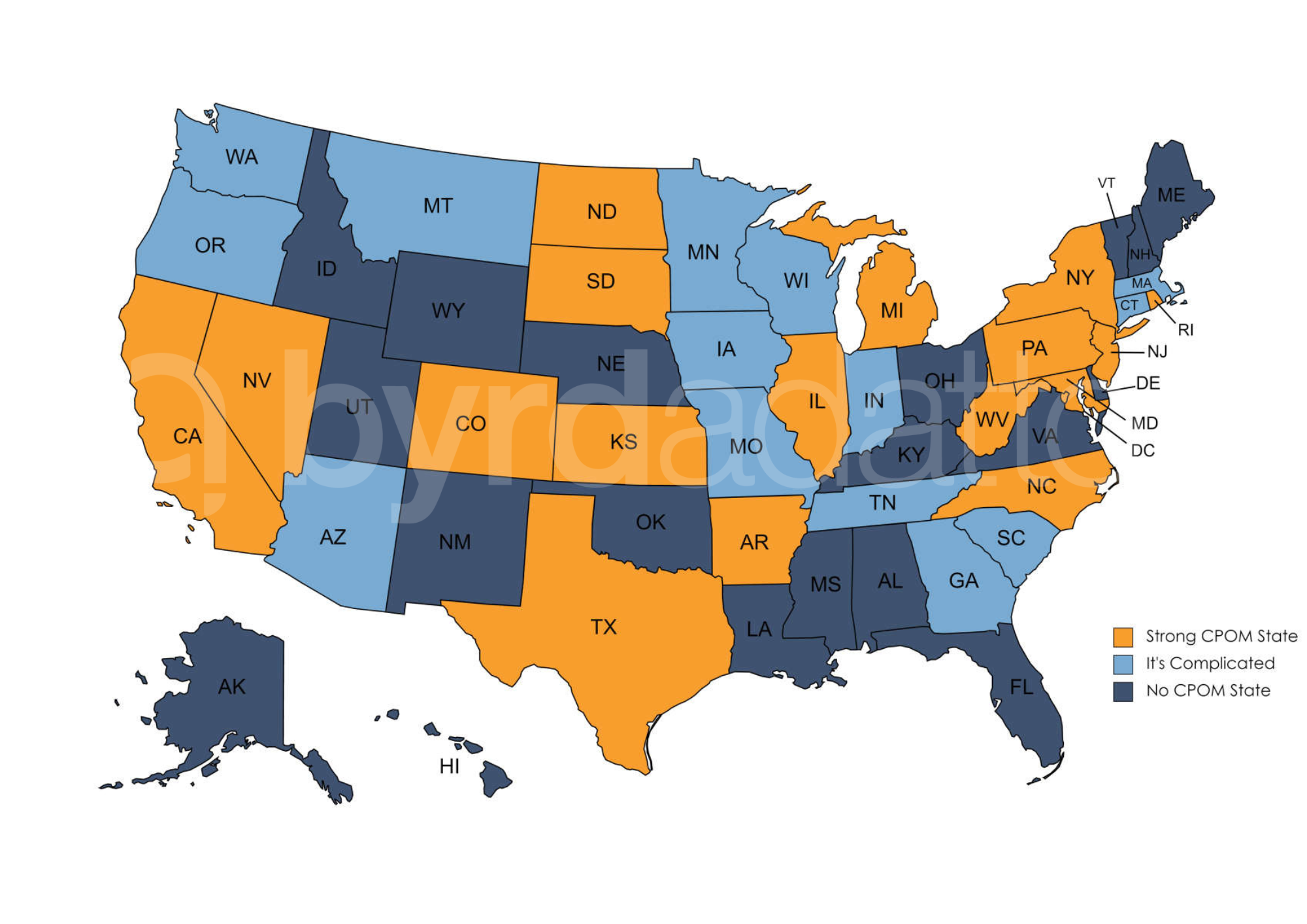
For illustration purposes, the CPOM map below paints the picture of where CPOM clearly exists, does not exist, and where the issue is complicated. Even among the states listed as “It’s complicated,” the laws vary significantly.
How Does an MSO Navigate CPOM?
The MSO navigates CPOM by allowing for a properly owned medical practice but separating out the non-clinical business operations into a non-professional entity that functions to provide management, administrative, and non-clinical support services. Under a contract called the management services agreement (MSA), the medical practice arranges for the services to be provided by the MSO.
The MSA establishes the boundaries to protect against a CPOM violation. At its simplest level, the MSA reserves all medical decision making to the physician owned medical entity and the business functions to the MSO. As we looked at in Part 1, the MSO may perform functions as limited as back office operations or as extensive as actually owning and leasing the practice assets and handling marketing. The services provided by the MSO typically include the provisions of space, intellectual property (licensing the brand and other trademarks), accounting, staffing, marketing and equipment. Importantly, the division between the two sides ensures that patient care itself will not be commercialized.
When carried out properly, the MSO therefore allows physicians access to the business support services they need and non-physicians ability to participate in a medical practice without either party running afoul of state limitations on CPOM. In states with a strict CPOM doctrine this approach is a necessity and in states that allow limited exceptions it offers a way to manage uncertainty as to how those exceptions might be applied.
What Are the Additional Guiding Principles to Navigate CPOM With the MSO Model?
CPOM dives deeper than ownership. The laws are designed to protect patients from non-physicians becoming involved with patient care. While the MSO model solves the ownership issue, additional principles should be followed. Although states will vary in their enforcement of CPOM, the following tend to be key principles to setting up an arrangement in a way that protects non-physicians from crossing the CPOM line:
- All medical decision-making must be by physicians;
- The physician must retain final authority to hire and fire clinical staff;
- All revenues for medical services must be paid to the medical practice; and
- Non-physicians must not have too much control over physicians.
All medical decision-making must be by physicians.
This is the biggest risk. The absentee physician is a threat to any business providing medical services. If a physician is being paid a fee to essentially lend the physician’s license to allow for the provision of medical services, everyone has serious compliance risk. The physician must be engaged and participate at the appropriate level from a state and standard of care perspective.
The physician must retain final authority to hire and fire clinical staff.
In Part 1, we mentioned that an MSO could have a role in clinical staff management, but this cannot take precedence over the physician running their own practice and making final choices on such staff. The physician must be involved in the hiring and firing process and have final authority over these decisions.
All revenues for medical services must be paid to the medical practice.
Patients and payers have a relationship to the medical provider, and it is that practitioner who is responsible for their own fees and the services they bill. The business entity may be hired to manage the billing and accounting but the professional entity is the actual collector of the fees. The medical practice then, through its own contract with the business entity that patients and payers have no part in, pays the business entity for its work.
Non-physicians must not have too much control over physicians.
This principle is a natural extension of the first two principles. Although states vary greatly on this principle, the general idea is that there are aspects on the business side of a medical practice that could impact patient care. Consequently, states create restrictions on non-physician control of these types of decisions. Examples of the types of decisions that many states require to be reserved to the physician are (1) medical equipment selection, (2) staffing the medical providers, and (3) marketing and advertising campaigns. Some state medical boards will even consider factors that create inappropriate economic control by the non-physician over the physician.
Contact ByrdAdatto
As discussed in Part 1, form and substance remains critical to a successful MSO. Both the medical practice and MSO must conduct their relationship in a manner that is consistent with the limitations in the MSA and within the boundaries of the applicable CPOM laws. In the day-to-day running of practice operations, it is easy to drift from contract terms and into non-compliance. The antidote is intentionality on compliance with the MSA. Successful MSOs evaluate their MSA on an annual basis to check in on compliance and make any amendments needed to adapt to the evolution of the business operations and relationship.
In Part 3 of this series we will discuss the regulatory uses that MSOs play in health care arrangements. If you have any questions or if you would like to learn more about MSOs, email us at info@byrdadatto.com.
